


Medically Reviewed By Margaret Etudo. Written By The Vitamins For Woman Team.
Struggling with vaginal dryness, pain, or recurrent UTIs after menopause? Learn how to get lasting relief from hormonal and natural evidence-based GSM treatments.
For many women over 45, menopause brings more than hot flashes and night sweats. One of the lesser-discussed but deeply impactful conditions is Genitourinary Syndrome of Menopause (GSM), formerly known as vaginal atrophy.
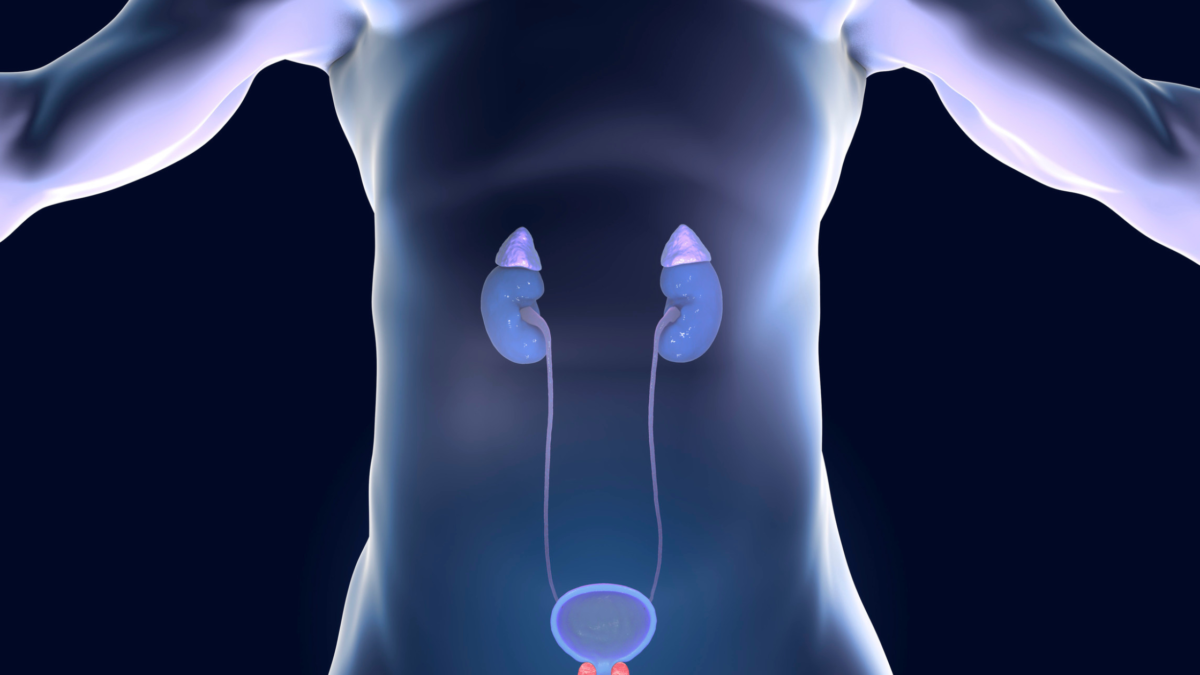
GSM includes a constellation of symptoms stemming from estrogen decline and affects the vaginal and urinary systems.
While it’s a natural part of aging, GSM is treatable. And yet, many women don’t seek help—either because they’re unaware it’s a medical issue or they believe it’s untreatable. As a pharmacist, I’m committed to bridging that knowledge gap.
This comprehensive guide explores the best GSM treatments, non-hormonal options, natural remedies, and answers to frequently asked questions.
Genitourinary Syndrome of Menopause is a clinical term used to describe the vaginal and urinary symptoms associated with reduced estrogen levels in menopause. It affects vaginal health, bladder function, and sexual comfort.
These symptoms are progressive, meaning they typically worsen without intervention.
Estrogen plays a crucial role in maintaining the elasticity, thickness, and moisture of vaginal tissues. After menopause, estrogen production significantly drops, leading to thinning of the vaginal walls, decreased lubrication, and changes in urinary tract tissues. This estrogen deficiency is the primary driver behind GSM.
What works best depends on your symptoms and what feels right for you. Here are some of the most trusted, research-backed treatments for vaginal dryness in 2025:
Vaginal estrogen therapy remains the gold standard for moderate to severe GSM treatment. It delivers low-dose estrogen directly to vaginal tissues, restoring thickness and lubrication while minimizing systemic absorption.
These options effectively reverse vaginal atrophy with minimal systemic risk. Vaginal estrogen also reduces the risk of recurrent UTIs.
Note: These therapies are not suitable for women with a history of hormone-sensitive cancers without physician oversight.
Hyaluronic acid is a naturally occurring molecule known for its water-retaining properties. Hyaluronic acid suppositories help keep the vagina hydrated and support healing—without using hormones. That makes them a great choice if you’re looking for a non-hormonal way to ease dryness and discomfort.
Studies show they really can make a difference. Just be sure to choose a high-quality product from a pharmacy or a trusted online store.
This GSM laser therapy uses fractional CO2 laser energy to stimulate collagen production and rejuvenate vaginal tissues. It is a non-hormonal outpatient procedure typically performed in 3 sessions over 12 weeks.
While more expensive, it’s a valuable option for women unable or unwilling to use hormones.
Unlike lubricants, vaginal moisturizers are used regularly, twice or thrice weekly, to maintain vaginal hydration. Look for products free from parabens, fragrances, and glycerin.
DHEA (dehydroepiandrosterone) inserts convert to estrogen and testosterone locally within the vaginal tissue. Prasterone (Intrarosa) is FDA-approved for GSM and offers hormonal benefits without significantly increasing serum hormone levels.
This oral medication is a Selective Estrogen Receptor Modulator (SERM) approved for dyspareunia due to GSM. It improves vaginal tissue integrity systemically.
For immediate symptom relief during intercourse, water- or silicone-based lubricants can reduce pain and friction. These do not treat GSM but improve sexual comfort.
Some women prefer or require non-hormonal GSM options, especially those with contraindications to hormone therapy. Natural remedies can be a valuable part of a holistic approach.
Vitamin E oil applied vaginally may help improve tissue integrity and reduce dryness. It acts as an antioxidant and promotes healing. Use pharmaceutical-grade suppositories or oils specifically designed for vaginal use.
Pelvic floor dysfunction can exacerbate GSM symptoms. Pelvic floor physical therapy improves blood flow, muscle tone, and urinary control. It’s beneficial for women experiencing urinary incontinence or painful intercourse.
Yes. GSM is a chronic condition. Stopping treatment often leads to the return of symptoms. Long-term maintenance therapy is typically required.
Absolutely. Options like hyaluronic acid suppositories, vaginal moisturizers, Mona Lisa Touch laser, and pelvic floor therapy offer effective non-hormonal GSM options.
Yes. When estrogen levels drop, it can change the lining and pH of the urinary tract, making it easier for infections to happen repeatedly. For many postmenopausal women, using a low-dose estrogen treatment right where it’s needed can help cut down on repeated UTIs.
GSM is common, progressive, and treatable. If you’re experiencing vaginal dryness, painful sex, or UTIs, you’re not alone—and you don’t have to suffer in silence.
Whether you’re seeking hormonal or non-hormonal GSM treatment, a wide array of effective options exist in 2025.
As a pharmacist, I encourage open conversations with your healthcare provider about what you’re experiencing. Relief is possible, and reclaiming your comfort, intimacy, and quality of life is well within reach.
Carlson K, Nguyen H. Genitourinary syndrome of menopause. In: StatPearls. StatPearls Publishing; 2025.
YPF: Genitourinary syndrome of menopause(Gsm). Your Pelvic Floor.
Rahn DD, Carberry C, Sanses TV, et al. Vaginal estrogen for genitourinary syndrome of menopause: a systematic review. Obstetrics and gynecology. 2014;124(6):1147.
Gold D, Nicolay L, Avian A, et al. Vaginal laser therapy versus hyaluronic acid suppositories for women with symptoms of urogenital atrophy after treatment for breast cancer: A randomized controlled trial. Maturitas. 2023;167:1-7.
Papakonstantinou E, Roth M, Karakiulakis G. Hyaluronic acid: A key molecule in skin aging. Dermato-endocrinology. 2012;4(3):253.
Best vaginal rejuvenation rancho cucamonga | channell wellness & aesthetics. Channell, Patricia (channellmedicalgroup.com).
Sarmento ACA, Kamilos MF, Costa APF, Vieira-Baptista P, José Eleutério J, Gonçalves AK. Use of moisturizers and lubricants for vulvovaginal atrophy. Frontiers in Reproductive Health. 2021;3:781353.
Zhou Y, Kang J, Chen D, Han N, Ma H. Ample evidence: dehydroepiandrosterone (Dhea) conversion into activated steroid hormones occurs in adrenal and ovary in female rat. PLoS ONE. 2015;10(5):e0124511.
Pan M, Zhou J, Pan X, Wang J, Qi Q, Wang L. Drugs for the treatment of postmenopausal symptoms: Hormonal and non-hormonal therapy. Life Sciences. 2023;312:121255.
Kennedy CE, Yeh PT, Li J, Gonsalves L, Narasimhan M. Lubricants for the promotion of sexual health and well-being: a systematic review. Sexual and Reproductive Health Matters. 2022;29(3):2044198.

medically reviewed by margaret etudo, BPharm. written by the vitamins for woman team.